Obstructive Sleep Apnea Severity: A Closer Look
A lot of folks with a milder case of obstructive sleep apnea (OSA) wonder if it’s worth treating.
Does severity matter? And do the symptoms, treatments, and risk factors differ between mild, moderate, or severe cases?
In order to understand severity, you need to understand how it’s defined.
Apnea-Hypopnea Index (AHI) basics
The Apnea-Hypopnea Index (AHI), also known as your AHI score, objectively measures the number of respiratory events you average per hour of sleep during a home-based or lab-based sleep study.
Respiratory events describe instances disrupted breathing during sleep, potentially leading to hypoxia or hypoxemia.
Hypoxia indicates a temporary dip in blood oxygen, which could mean 1 to 2 percent within the range of normal, or a larger dip from normal to below normal.
Hypoxemia, on the other hand, indicates a blood oxygen level maintained over time that remains below what’s considered safe and normal. What’s normal? Above 90 percent.
3 kinds of respiratory events
A sleep test measures 3 kinds of respiratory events: apneas, hypopneas, and respiratory effort-related arousals. Here is how the American Academy of Sleep Medicine defines these.1
1. Apneas
The term apnea literally means “no breath.” In OSA, these are complete pauses in breathing caused by obstructions. They last at least 10 seconds and can persist for 30 seconds or longer. Meanwhile, the body continues to make an effort to breathe.
Usually, arousals of sleep mark an apnea’s end; these arousals occur as a result of several mechanisms in the body designed to protect you against hypoxia. A drop of between 3 and 4 percent of one’s blood oxygen is concerning, as these drops can lead to hypoxemia.
2. Hypopneas
The term hypopnea literally means “under breath.” In OSA, these are partial pauses in breathing caused by obstructions. These pauses may restrict anywhere from 30 to 90 percent of airflow and last at least 10 seconds.
A drop of between 3 and 4 percent of one’s blood oxygen is concerning, as these drops can lead to hypoxemia.
3. Respiratory effort-related arousals (RERAS)
In OSA, these are breathing disruptions that occur during sleep which don’t satisfy the definition of apnea or hypopnea, but which do contribute to frequent arousals during sleep (sleep fragmentation).
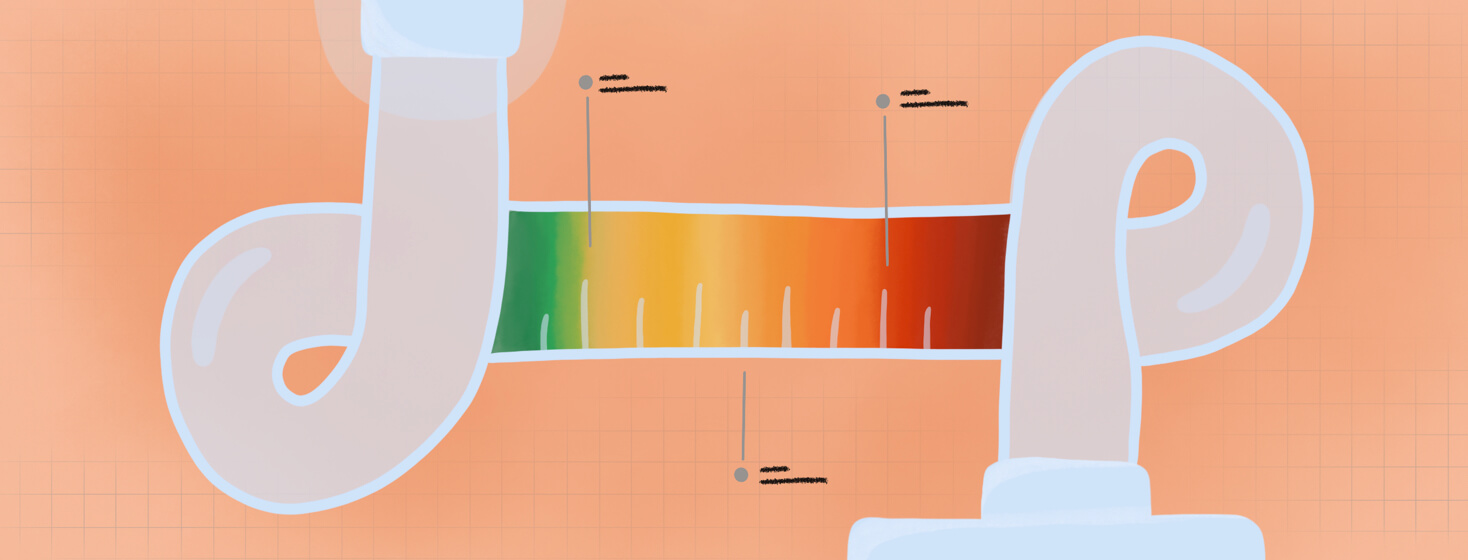
The OSA severity scale
Let’s take a closer look at severity levels as defined by the American Academy of Sleep Medicine.1
- Mild OSA – Averaging between 5 and 15 respiratory events per hour. Really important! Mild OSA isn’t the same as no OSA. Mild OSA still poses the same risks to the human body if left untreated.
- Moderate OSA – Averaging between 15 and 30 respiratory events per hour.
- Severe OSA – Averaging more than 30 respiratory events per hour.
Differences in symptoms and OSA severity
Common sense suggests that the more severe the OSA, the more severe the symptoms. However, AHI severity doesn’t always correlate with symptoms. Some with a low AHI can be extremely symptomatic, while others with a high AHI may feel they sleep great and don’t report daytime fatigue.2
But people of all OSA severities can experience any or all of the symptoms of untreated OSA.3-5
Nighttime symptoms
- Loud and/or frequent snoring
- Silent pauses in breathing
- Noisy recovery (choking or gasping)
- Tossing and turning
- Frequent periods of nighttime sleeplessness
- Frequent bathroom breaks
- Night sweats
- Enuresis (bedwetting) in children and adults
Daytime symptoms
- Excessive daytime sleepiness (EDS)
- Waking up feeling unrefreshed
- Morning headaches
- Morning dry mouth or sore throat
- Difficulty concentrating
- Memory loss
- Decreases sexual desire
- Erectile dysfunction
- Irritability
- Drowsy driving in adults
- Poor school performance in children/job performance in adults
- Visible mouth breathing
Differences in treatments and OSA severity
Following an OSA diagnosis, most people are introduced to positive airway pressure (PAP) therapy:
- Continuous PAP (CPAP)
- Bilevel PAP (BiPAP)
- Automatic PAP (autoPAP)
PAP therapy remains the industry gold standard for treating OSA, as it’s the most consistently effective treatment for OSA.1,6
However, not everyone responds well to PAP, even when they have mild OSA. Other options include:1,7
- Positional therapy
- Weight loss
- Oral appliance therapy
- Other noninvasive ventilation technologies: adaptive servo-ventilation (ASV) or average volume-assured pressured support (AVAPS)
- Combination of oral appliance and PAP
- Combination of PAP and oxygen supplementation
- Hypoglossal nerve stimulation implant
- Surgical procedures
For some, a combination of approaches may work best.
Differences in risk factors and OSA severity
The following factors increase your risk of developing sleep apnea at every severity level.1,7,8
- Being overweight or obese (body mass index of 25 or higher)
- Having a thicker neck (includes those with a low body-mass index or BMI, such as body builders)
- Narrow airways due to the physical features of your jaw, soft tissues (adenoids, tongue, tonsils, uvula)
- Male gender
- Higher age
- Post-menopausal women
- Family history
- Substance use (alcohol, sedatives, tranquilizers, nicotine)
- Chronic nasal congestion
- Comorbid conditions: heart disease, high blood pressure, type 2 diabetes, Parkinson’s disease, asthma, polycystic ovary syndrome, prior stroke, hormone disorders, Down Syndrome, acromegaly, hypothyroidism
The bottom line?
It’s important to note that OSA doesn’t have a cure; no matter how severe the case, it requires treatment.
Join the conversation